Akiko Iwasaki is a Professor of Immunology at Yale and a former student in my department (Dept. of Biochemistry, University of Toronto). She got her undergraduate degree in biochemistry in the mid-1990s1 and then did her Ph.D. in the Dept. of Imunology under my friend and colleague Brian Barber.
Alex Pallazzo is a keen podcast listener and he alerted me to an interview with Akiko Iwasaki on the EMBO podcast channel: The Right Place at the Right time. There are several reasons why listening to this podcast is worthwhile if you are interested in science and immunology. The most important reason is that it gives you a good idea of the depth of knowledge in the field because the level of the interview is pitched at those who have a considerable understanding of imunology. I'm not one of those people but I recognize good science when I hear it.
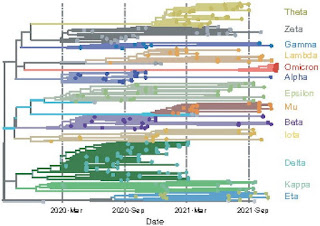
Another reason is that she discusses COVID-19 and how vaccines work. As you know from earlier posts, the serum antibody levels induced by the current vaccines wane after a few months so that vaccinated people can get infected by the SARS-CoV-2 virus. The secondary response then kicks in protecting you from serious illness. In order to stop the initial infections and prevent the spread of the virus we might have to get booster shots every six months or so and that's not a satisfactory solution.
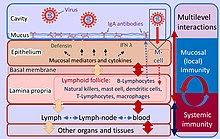
Iwasaki works on something called mucosal immunity, which is new to me but very familiar to the experts. Here's a brief description from her website and a figure from Wikipedia.
The mucosal surfaces represent major sites of entry for numerous infectious agents. Consequently, the vast mucosal surfaces are intricately lined with cells and lymphoid organs specialized in providing protective antibody and cellular immunity. One of the most fundamental issues in this field concerns how antigens in the mucosa are taken up, processed, and presented by antigen presenting cells. Our laboratory's goal is to understand how immunity is initiated and maintained at the mucosal surfaces, particularly by the dendritic cells (DCs), through natural portals of entry for pathogens that are of significant health concerns in the world.
We focus on understanding how viruses are recognized (innate immunity) and how that information is used to generate protective adaptive immunity.
I hope I understand this well enough to explain it in simple terms. Mucosal immunity means that there are IgA antibodies in the mucosa that surrounds cells in certain parts of the body. For our purposes, the cells in the respiratory tract are important in COVID-19. The memory B-cells and T-cells that respond to the antigen are located right under the mucosa. Imagine that you could produce a vaccine that induced IgA against SARS-CoV-2 in the mucosa. The antibodies would be located right where the virus enters the body and they don't disappear over time like IgG in the blood stream. Furthermore, the secondary response is induced right near the site where the virus is attacking the body.
I think you need a nasal/throat spray vaccine to make this work and such vaccines are under development. They would probably have to be given in conjunction with the intra-muscular mRNA vaccines. I wish I could get Brian Barber to explain this but I can't seem to contact him. He gave a short lesson in immunology on his daughter, Jill Barber's Instagram account last year so I know he could do it.
I learned one other thing from listening to Akiko Iwasaki. We know that SARS-CoV-2 is more virulent in cold weather, especially during the winter months. She explains that the mucosal layer needs to be kept moist but during the winter months it can dry up due to the low humidity. The outside air is cold, therefore the humidity is low, and we import that air into our homes and workplaces. This dry air promotes spread of the virus.
Maybe we should be installing extra humidifiers to keep the humidity at higher levels?
It's a bit of a stretch from Akiko Iwasaki to Jill Barber but we've known Jill since she was little and my wife and I are big fans so here's a musical interlude to take your mind off COVID-19.
1. She must have taken my Molecular biology course and that's probably why she knows so much!